Lectins have become one of the more debated food compounds in recent years, not because they suddenly appeared in the human diet, but because people are beginning to notice that these natural proteins don’t affect everyone the same way. While many individuals can consume beans, grains, nuts, and nightshade vegetables with no noticeable issues, others report digestive discomfort, fatigue, joint pain, rashes, or brain fog after meals containing high-lectin ingredients. This difference in reactions has raised an important question: why do some bodies tolerate lectins effortlessly while others seem immediately irritated by them?
The answer is not simple. It involves genetics, gut microbiome composition, digestive efficiency, immune sensitivity, and even the body’s past experiences with inflammation. Understanding these layers doesn’t just explain symptoms. It helps people make more personalized decisions about their diet.
A Universal Protein With a Highly Individual Response
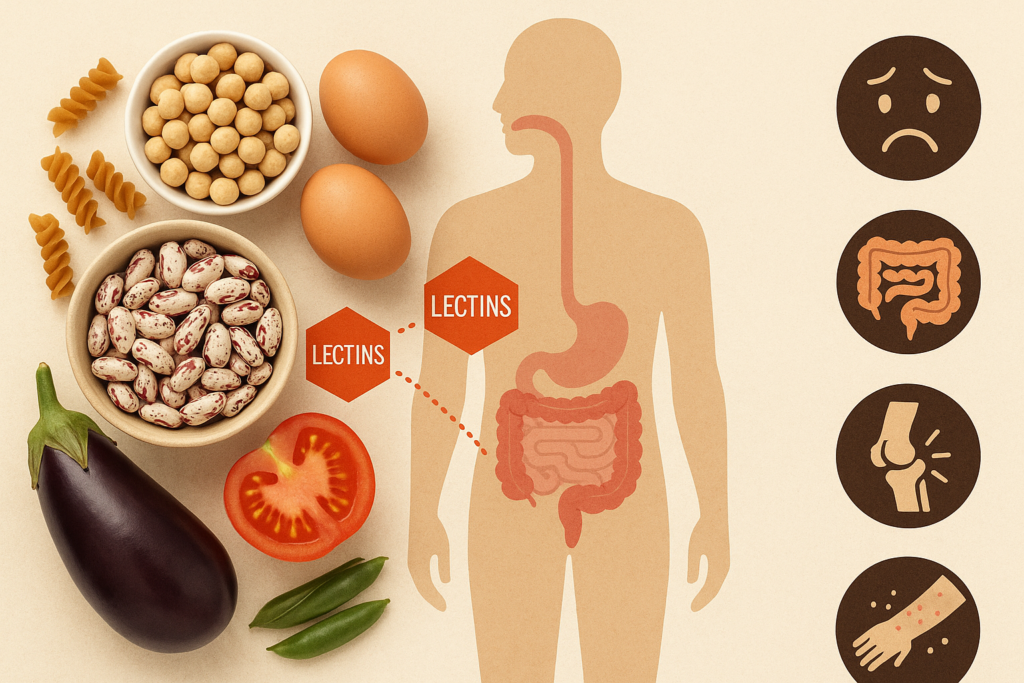
Lectins are a type of protein found in many plants. Their natural purpose is defensive. Plants can’t run away from predators, so they evolved biochemical ways to discourage insects, fungi, and animals from eating them. Lectins can bind to carbohydrates on the surface of cells, which in nature helps protect the plant. In humans, this same carbohydrate-binding behavior sometimes irritates the lining of the gut or disrupts digestion. But whether that irritation becomes a noticeable problem depends on dozens of internal variables that differ wildly from person to person.
In other words, lectins are universal, they’re in many foods but the human response to them is not. Some people break them down efficiently. Some people have microbiomes that neutralize them. Others have immune systems primed to overreact. And a few may not notice them at all unless extremely high amounts are consumed.
The Gut Barrier: The First Line of Defense
One of the strongest predictors of lectin sensitivity is the condition of the gut barrier. Picture the gut lining as a selectively permeable wall, built with tightly arranged cells meant to allow nutrients through while keeping unwanted molecules out. When it’s healthy, lectins are just another compound passing through digestion with minimal interaction.
But if the intestinal barrier becomes compromised, sometimes referred to as increased intestinal permeability, lectins have more direct contact with the underlying immune system. This can magnify any reaction, even if the person never had trouble with lectins before.
Several factors can weaken this barrier:
- Chronic stress
- Heavy alcohol consumption
- Long-term NSAID use
- Certain infections
- Diets high in refined sugar
- Previous inflammatory bowel issues
When the gut is already irritated, lectins don’t have to do much to cause discomfort. They simply become one more irritant in an already overwhelmed system, which is why some individuals notice reactions only during specific periods of their life like after illness, during intense stress, or following major dietary disruptions.
Microbiome Differences: The Hidden Variable
If the gut lining is the barrier, the gut microbiome is the internal task force managing digestion. trillions of bacteria, fungi, and other microorganisms help break down complex foods, including lectin-rich ingredients. But every person’s gut microbiome is unique, more like a fingerprint than a universal template.
Some microbes degrade lectins efficiently, neutralizing their potential irritant effects. Certain strains of beneficial bacteria even prefer lectin-bearing foods, helping reduce reactions before they ever reach the immune system.
But if someone has a depleted or imbalanced microbiome, often due to antibiotics, chronic stress, poor diet, or illness, lectins can linger longer during digestion, interact more strongly with the gut lining, and generate more noticeable symptoms.
This explains why two people can eat the exact same lectin-rich chili or bean salad and have completely opposite experiences. To one person, it’s a satisfying meal. To the other, it’s bloating, cramping, and fatigue. Their microbiomes simply don’t process lectins the same way.
Genetics: The Blueprint Behind Sensitivity
Beyond gut health, genetics also play a role in determining who reacts to lectins. Although research is still emerging, scientists have identified several genetic factors that may influence lectin tolerance:
- Variations in digestive enzyme production can affect the breakdown of plant proteins.
- Differences in immune system receptors can lead some people to respond more aggressively to certain food compounds.
- Genes related to gut barrier formation may influence the strength or resilience of the intestinal lining.
Genetics don’t determine lectin sensitivity outright, but they shape a person’s biological baseline. Two individuals may follow the same diet and lifestyle but inherit different digestive characteristics that influence whether lectins feel harmless or irritating.
Immune System Sensitivity: How Reactivity Builds Over Time
The immune system is constantly evaluating what comes through the digestive tract. Most of the time, it ignores food particles entirely, recognizing them as harmless. But in some people, the immune system becomes hyper-vigilant, reacting to proteins that ordinarily wouldn’t trigger a response.
Lectins have a structure that can sometimes catch the immune system’s attention, especially in individuals with:
- Autoimmune tendencies
- Chronic inflammatory conditions
- Past gastrointestinal infections
- Histamine intolerance
- High inflammatory load from unrelated dietary issues
For these individuals, lectins can act like a spark landing in a pile of tinder. The lectin itself isn’t “attacking” anything, but it can provoke an immune response simply because the immune system is already on high alert.
The relationship between lectins and the immune system isn’t identical to an allergy. It doesn’t always involve classic immune pathways but it does highlight how a person’s internal environment determines their tolerance.
Digestive Capability: Not Everyone Produces the Same Tools
Digestion isn’t just chewing and swallowing; it’s a coordinated system involving stomach acid, enzymes, bile, and microbial fermentation. If any part of this process is impaired, lectins may pass through the digestive system more intact and more capable of interacting with the gut lining.
Several digestive factors influence how someone reacts to lectins:
Stomach Acid Levels – Low stomach acid (a surprisingly common issue) allows proteins to enter the small intestine less broken down than they should be. When this happens, lectins may behave more aggressively.
Enzyme Availability – Some people produce more robust protein-breaking enzymes than others. When enzyme levels drop, lectins remain more active during digestion.
Transit Time – Slow digestion increases exposure time. Lectins that linger in the gut have more opportunity to cause irritation.
Digestive capability can shift with age, medication, illness, and stress, which is why someone who once tolerated certain foods easily might later find they no longer can.
Cooking Techniques and Their Role in Sensitivity
One of the most overlooked reasons why people experience different reactions to lectins is simple: not everyone cooks high-lectin foods the same way.
Lectins in beans, legumes, and some grains can be dramatically reduced through proper preparation:
- Soaking
- Rinsing
- Pressure cooking
- Fermenting
- Extended boiling at sufficient temperatures
If someone grows up in a household or culture that uses these methods, they may consume lectin-rich foods without issue. But if another person eats the same foods without adequate cooking, for example beans cooked too quickly or pressure-cooked without soaking, their experience might be entirely different.
Cooking isn’t just culinary tradition; it’s biochemical transformation. The same ingredient can behave differently depending on how it’s prepared.
Previous Diet and Exposure: The Body Remembers
A person’s history with food affects how they react to lectins today. Someone who spent years eating a heavily processed diet, dealing with frequent antibiotics, or living through prolonged inflammation may simply have a more delicate digestive system.
On the other hand, someone who regularly ate whole foods from childhood, including lectin-rich foods, may have a microbiome better adapted to breaking them down. Their digestive system essentially “grew up” with these compounds.
This adaptive aspect explains why some people experience lectin issues only after switching diets. If they move abruptly from processed foods to a whole-food diet rich in beans, grains, nuts, and vegetables, the sudden influx of lectins may overwhelm a system that never learned to handle them.
Stress and Hormonal Influences: The Quiet Disruptors
Stress hormones directly affect digestion. They alter stomach acid, slow down or speed up gut motility, and influence the microbiome. Stress can also trigger or worsen inflammation, reduce sleep quality, and weaken the gut barrier.
If someone is under chronic stress, lectins don’t necessarily become the problem. The body’s ability to process them does.
This also applies to hormonal fluctuations, such as those seen during menstruation, perimenopause, chronic endocrine disorders, or thyroid imbalances. Hormones affect nearly every regulatory system in the gut, which means sensitivity to lectins can vary throughout life.
The Threshold Effect: A Little Is Fine, Until It Isn’t
Lectin sensitivity is rarely absolute. Most people aren’t reacting to every gram of lectins they consume. Instead, they have a threshold, an amount they can handle without symptoms. When they exceed that threshold, reactions begin.
This threshold varies depending on:
- The combination of foods eaten that day
- The current condition of the gut
- Stress levels
- Sleep quality
- Hydration
- Immune activation
For example, someone might tolerate tomatoes well when their stress levels are low and their digestion is functioning optimally, but react after a stressful week coupled with poor sleep. Another person may tolerate beans only when pressure-cooked and eaten in moderate portions, but not in larger quantities.
Thresholds make lectin reactions seem unpredictable, but they are actually a reflection of the body’s daily resilience.
Individual Variation Doesn’t Mean Lectins Are Inherently Harmful
One of the most important things to understand is that lectins themselves are not universally dangerous. Entire cultures around the world rely on lectin-rich foods like lentils, chickpeas, peanuts, tomatoes, eggplants, and whole grains without experiencing widespread digestive issues.
The variability in human response is the real story here. Lectin sensitivity is not a judgment on the food; it’s a clue about the state of the body that consumes it.
Some people tolerate lectins because their microbiome, digestion, immune system, and cooking techniques all support that tolerance. Others react because one or more of those systems is strained, imbalanced, or genetically predisposed to sensitivity.
Recognizing this distinction allows individuals to make dietary choices based on personal observation rather than blanket rules.
Finding Your Own Lectin Tolerance Level
If someone suspects they are reacting to lectins, the goal is not to eliminate every lectin-bearing food forever. Instead, the goal is to learn how their body responds and adjust accordingly. This may involve:
Trying pressure-cooked versions of foods that previously caused issues
Avoiding raw or undercooked high-lectin ingredients
Supporting the gut microbiome through fermented foods
Working on stress, hydration, sleep, and overall lifestyle
Reintroducing foods slowly after a break to assess tolerance
Every body has its own threshold, and discovering it is a process of careful observation rather than permanent restriction.
Conclusion: A Personalized Perspective on Lectins
Why some people react to lectins more than others is ultimately a story about individuality, the uniqueness of each person’s gut, immune system, genetics, microbiome, and life experiences. Lectins are not inherently harmful, but they can become problematic in the wrong environment or in a system already under strain.
For some people, reducing lectins gives their body space to heal. For others, lectins pose no issue at all. Understanding the factors behind lectin sensitivity empowers individuals to make decisions based not on fear, but on informed self-awareness.
The more we learn about the relationship between lectins and the human body, the clearer it becomes that tolerance is not universal. It is personal, adaptable, and deeply tied to the overall health of the digestive and immune systems.